What is Hep B and how effective is vaccination.
What is Hepatitis B?
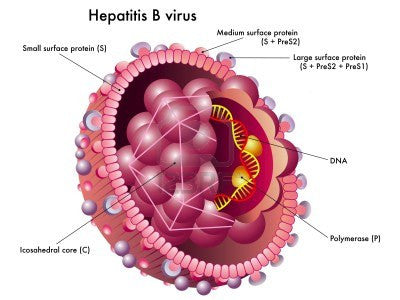
Hepatitis B is an infection caused by the hepatitis B virus (HBV), which is transmitted through percutaneous (i.e., breaks in the skin) or mucosal (i.e., direct contact with mucous membranes) exposure to infectious blood or body fluids. The virus is highly infectious; for nonimmune persons, disease transmission from a needlestick exposure is up to 100 times more likely for exposure to hepatitis B e antigen (HBeAg)--positive blood than to HIV-positive blood (14).
HBV infection is a well recognized occupational risk for U.S. HCP and globally. The risk for HBV is associated with degree of contact with blood in the work place and with the hepatitis B e-antigen status of the source persons (15). The virus is also environmentally stable, remaining infectious on environmental surfaces for at least 7 days (16).
In 2009 in the United States, 3,371 cases of acute HBV infection were reported nationally, and an estimated 38,000 new cases of HBV infection occurred after accounting for underreporting and underdiagnosis (17). Of 4,519 persons reported with acute HBV infection in 2007, approximately 40% were hospitalized and 1.5% died (18). HBV can lead to chronic infection, which can result in cirrhosis of the liver, liver failure, liver cancer, and death.
An estimated 800,000--1.4 million persons in the United States are living with chronic HBV infection; these persons serve as the main reservoir for continued HBV transmission (19).
Hepatitis B Vaccine Info
Vaccines to prevent hepatitis B became available in the United States in 1981; a decade later, a national strategy to eliminate HBV infection was implemented, and the routine vaccination of children was recommended (20). During 1990--2009, the rate of new HBV infections declined approximately 84%, from 8.5 to 1.1 cases per 100,000 population (17); the decline was greatest (98%) among persons aged <19 years, for whom recommendations for routine infant and adolescent vaccination have been applied. Although hepatitis B vaccine coverage is high in infants, children, and adolescents (91.8% in infants aged 19--35 months and 91.6% in adolescents aged 13--17 years) (21,22), coverage remains lower (41.8% in 2009) for certain adult populations, including those with behavioral risks for HBV infection (e.g., men who have sex with men and persons who use injection drugs) (23).
How Effective is the Hepatitis B Vaccine?
The 3-dose vaccine series administered intramuscularly at 0, 1, and 6 months produces a protective antibody response in approximately 30%--55% of healthy adults aged ≤40 years after the first dose, 75% after the second dose, and >90% after the third dose (40--42). After age 40 years, <90% of persons vaccinated with 3 doses have a protective antibody response, and by age 60 years, protective levels of antibody develop in approximately 75% of vaccinated persons (43). Smoking, obesity, genetic factors, and immune suppression also are associated with diminished immune response to hepatitis B vaccination (43--46).
How long with immunity last after Vaccination?
Protection against symptomatic and chronic HBV infection has been documented to persist for ≥22 years in vaccine responders.
Hepatitis B for Healthcare employees
During 1982, when hepatitis B vaccine was first recommended for HCP, an estimated 10,000 infections occurred among persons employed in a medical or dental field. By 2004, the number of HBV infections among HCP had decreased to an estimated 304 infections, largely resulting from the implementation of routine preexposure vaccination and improved infection-control precautions (24--26).
The risk for acquiring HBV infection from occupational exposures is dependent on the frequency of percutaneous and mucosal exposures to blood or body fluids (e.g., semen, saliva, and wound exudates) containing HBV, particularly fluids containing HBeAg (a marker for high HBV replication and viral load) (27--31). The risk is higher during the professional training period and can vary throughout a person's career (1). Depending on the tasks performed, health-care or public safety personnel might be at risk for HBV exposure; in addition, personnel providing care and assistance to persons in outpatient settings and those residing in long-term--care facilities (e.g., assisted living) might be at risk for acquiring or facilitating transmission of HBV infection when they perform procedures that expose them to blood (e.g., assisted blood-glucose monitoring and wound care)
Other Considerations
Occupational health programs and others responsible for infection prevention and control should identify all staff whose work-related activities involve exposure to blood or other potentially infectious body fluids in a health-care, laboratory, public safety, or institutional setting (including employees, students, contractors, attending clinicians, emergency medical technicians, paramedics, and volunteers); provide education to staff to encourage vaccination; and implement active follow-up, with reminders to track completion of the vaccine series and postvaccination testing among persons receiving vaccination (72).
In partnership with state and local health authorities, household, sex, or needle-sharing contacts of HBsAg-positive HCP and trainees should be identified, tested, vaccinated (if indicated), and provided with counseling and referral for needed services, when appropriate.
Information from CDC
Hep B Transmission
Hepatitis B is found in blood and in body fluids, including semen and vaginal fluids. Even though studies have shown minute quantities of the virus can be present in saliva, tears and breast milk, they are not considered to be in high enough levels to transmit the virus.
The most common ways hepatitis B is spread include:
- sexual contact
- sharing of injecting equipment
- needlestick injuries in a health care setting
- reuse of unsterilised or inadequately sterilised needles
- child-to-child transmission through contact such as biting
- sharing personal items such as razors, toothbrushes, or hair and nail clippers
- mother-to-baby, though it is to be noted that the Australian vaccination program has significantly reduced this risk through the administration of the vaccine within 12 hours of birth.
Hepatitis B is NOT spread by contaminated food or water, and cannot be spread through casual or social contact such as kissing, sneezing or coughing, hugging, or eating food prepared by a person with hepatitis B.
Leave a comment: